Sudden cardiac arrest remains a major health crisis, and the statistics on survival rates underscore the extreme urgency of immediate, decisive action. For every minute that passes after a person collapses from cardiac arrest, their chances of survival drop significantly, making the first few moments absolutely crucial. In these critical situations, rapid intervention with defibrillation serves as a pivotal, life-saving emergency response. Defibrillation is not merely an isolated step; it is a critical electrical therapy designed to reset the heart’s electrical system when it has fallen into a lethal, chaotic rhythm. Understanding how and when to use this technology is essential for medical professionals and the public alike. This comprehensive guide will define defibrillation, explain its core purpose in reversing fatal heart rhythms, detail its crucial role within the larger context of cardiopulmonary resuscitation, and stress the importance of proper, hands-on training to master this life-altering procedure.
What is Defibrillation? Understanding the Basics
The core concept of defibrillation is rooted in electrical shock therapy applied directly to the chest. Medically, defibrillation is defined as the process of delivering a controlled electrical shock to a patient’s heart. This powerful, brief electrical current is not meant to restart a heart that is completely flatlined, but rather to momentarily “stun” the chaotic electrical activity of the heart muscle. By temporarily stopping all electrical activity, the shock provides the heart’s natural pacemaker with an opportunity to reorganize itself and take over, hopefully restoring a normal, effective heart rhythm. The science behind this is about interrupting electrical chaos and allowing for synchronized electrical function to return.
Types of Abnormal Heart Rhythms Treated
Defibrillation is an intervention specifically reserved for two particular types of abnormal heart rhythms that are often referred to as “shockable rhythms.” The first is ventricular fibrillation, widely known as V-fib, a disorganized state where the ventricles merely quiver uselessly instead of pumping blood effectively, which leads immediately to cardiac arrest. The second is pulseless ventricular tachycardia, or V-tach, a very fast, irregular rhythm that prevents the heart from filling with enough blood to maintain circulation. It is absolutely crucial to understand that defibrillation is not appropriate for every patient experiencing cardiac arrest; specifically, it is not used when the heart has no electrical activity at all, a rhythm known as asystole, or when the rhythm is organized but without a pulse. Effective treatment hinges on the correct identification of these specific shockable rhythms.
Primary Medical Applications
A defibrillator is used across many settings, primarily to treat sudden cardiac arrest. Its applications are broad, ranging from high-level emergency room and hospital use, where advanced medical teams deploy manual devices, to pre-hospital emergency medical services, where paramedics and EMTs rely on portable units. However, the use of defibrillators has been successfully extended beyond the professional setting through the widespread deployment of Automated External Defibrillators, or AEDs.
Different Types of Defibrillators
There are several different types of defibrillators, each designed for a specific setting and level of care. Automated External Defibrillators, or AEDs, are designed for public use, featuring simple voice prompts to guide lay rescuers through the process of rhythm analysis and shock delivery. Manual defibrillators are complex devices used by expert medical teams to allow for adjustable energy levels and advanced rhythm interpretation. Furthermore, patients with chronic heart conditions may have an Implantable Cardioverter Defibrillator, known as an ICD, surgically placed beneath the skin, or utilize a Wearable Cardioverter Defibrillator, which monitors the heart and delivers an immediate shock if a dangerous rhythm is detected without requiring any external action.
The Role of Defibrillation in CPR: A Crucial Partnership
The Chain of Survival
The application of defibrillation forms a crucial partnership with cardiopulmonary resuscitation and is a critical component of the Chain of Survival. This universally accepted concept outlines the ideal sequence of actions required to maximize a cardiac arrest victim’s chance of survival. The Chain begins with early recognition of the emergency and activation of emergency response systems. This is immediately followed by early, high-quality CPR, with a strong emphasis on chest compressions to keep blood flowing. The third and most critical link is rapid defibrillation, ensuring that the necessary electrical therapy is delivered as quickly as possible. The final links involve effective advanced life support delivered by medical personnel. Defibrillation integrates seamlessly into the CPR process; ideally, CPR should begin immediately upon recognizing cardiac arrest, and the shock should be delivered as soon as the defibrillator is ready. Importantly, CPR must also resume immediately after the shock delivery, minimizing any interruptions to chest compressions, as a continuous flow of oxygenated blood is the ultimate goal. Team coordination in this emergency response is key to performing rhythm analysis and shock delivery quickly and safely.
Call Us Now
Get the Best CPR Class in Indianapolis Today!
How Defibrillation Integrates with CPR
The integration of the AED and the CPR protocol is a defined process essential for all rescuers. When a person collapses, a rescuer initiates CPR, starting with chest compressions, while another rescuer prepares the AED. The AED pads are quickly attached to the patient’s bare chest, and the device performs its rhythm analysis. If the AED determines a shockable rhythm is present, it will advise a shock. The rescuer must clearly announce the intention to deliver a shock, ensuring safety considerations are met by confirming that no one is touching the patient during the shock delivery. Immediately after the shock is administered, the rescuer must restart chest compressions without delay, continuing the cycle until the patient recovers or advanced help takes over.
CPR vs. Defibrillation: Understanding the Key Differences
To fully appreciate this critical partnership, it is important to understand the fundamental differences between CPR and defibrillation.
CPR: Manual Life Support
CPR is purely a manual life support technique. Its purpose is to physically maintain blood circulation and oxygenation through the manual techniques of chest compressions and rescue breathing. CPR is initiated for any cardiac arrest or respiratory arrest, regardless of the underlying rhythm.
Defibrillation: Electrical Intervention
Defibrillation, conversely, is an electrical intervention. Its single purpose is to correct specific abnormal heart rhythms, namely V-fib and V-tach, using a controlled electrical shock. The mechanism involves rhythm analysis and shock delivery.
Why Both Are Essential
Both are essential and complementary roles in cardiac arrest response; neither replaces the other. The timing and coordination of these two interventions are what ultimately determine a positive outcome. The quick performance of chest compressions and the rapid delivery of a shock at the right time are the hallmarks of effective resuscitation.
FAQs About Defibrillation
1. How quickly should a defibrillator be used during cardiac arrest?
A defibrillator should be used as quickly as possible during sudden cardiac arrest. Every minute that passes without defibrillation reduces survival chances by approximately 7-10%. Ideally, defibrillation should occur within the first 3-5 minutes of cardiac arrest for the best outcomes. This is why having trained responders and accessible AEDs (Automated External Defibrillators) in public spaces is so critical to saving lives.
2. Can anyone use an AED, or do you need special training?
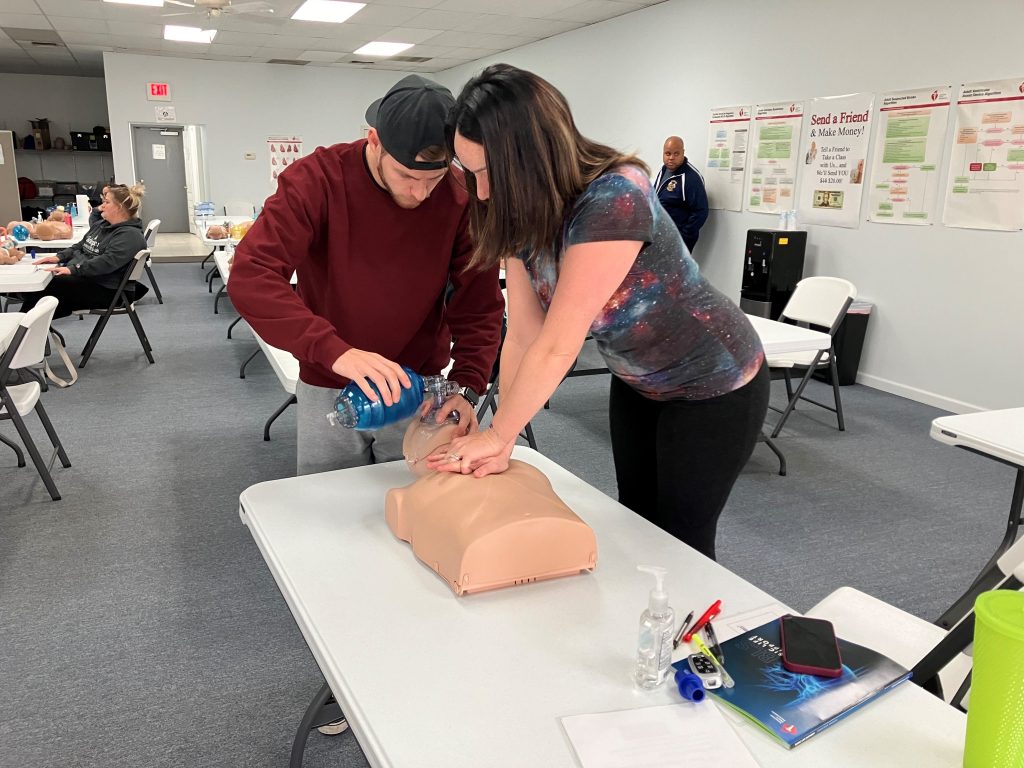
AEDs are specifically designed to be user-friendly so that anyone can operate them in an emergency, even without prior training. The device provides clear voice prompts and visual instructions to guide users through each step. However, proper training through BLS or CPR certification courses significantly increases confidence and effectiveness in emergency situations, ensuring you can respond quickly and correctly when every second counts.
3. What’s the difference between defibrillation and CPR?
Defibrillation and CPR work together but serve different purposes. Defibrillation delivers an electrical shock to restore a normal heart rhythm when the heart is in a life-threatening arrhythmia like ventricular fibrillation. CPR (cardiopulmonary resuscitation) manually pumps blood through the body to maintain circulation and oxygen flow to vital organs. CPR should be performed immediately while waiting for a defibrillator to arrive, and continued between shocks as needed.
4. Are defibrillators safe to use on children and infants?
Yes, defibrillators can be safely used on children and infants, though the approach differs slightly. Many AEDs have pediatric pads or a pediatric mode that delivers a lower energy shock appropriate for children under 8 years old or weighing less than 55 pounds. For infants under one year, manual defibrillators operated by healthcare professionals are preferred. Training in PALS (Pediatric Advanced Life Support) provides specialized knowledge for treating pediatric cardiac emergencies.
Call to Action
Don’t wait for an emergency to learn these life-saving skills. Enroll in CPR certification in Indianapolis or BLS classes in Indianapolis today at CPR Indianapolis, an American Heart Association training site. Our hands-on, stress-free courses will give you the confidence and competence to respond effectively when someone’s life is on the line. Visit us to register for BLS for Healthcare Providers, ACLS, PALS, or CPR and First Aid courses—because being prepared can make all the difference.


